Priorities for Stroke Rehabilitation

Payas Sinha
July 31, 2021
A post looking at the key priority areas for stroke rehabilitation, as identified by the Stroke Association in the Stroke Priority Setting Partnership.

Welcome!
Hi all! In this post, we are focusing on priority areas for stroke rehabilitation and long-term care.
For those who may not know, stroke is a condition in which blood supply to part of the brain is reduced or completely cut-off. 1 in 5 people will have a stroke in their lifetime, and it is a leading cause of death and disability in the UK1.
What is this post about?
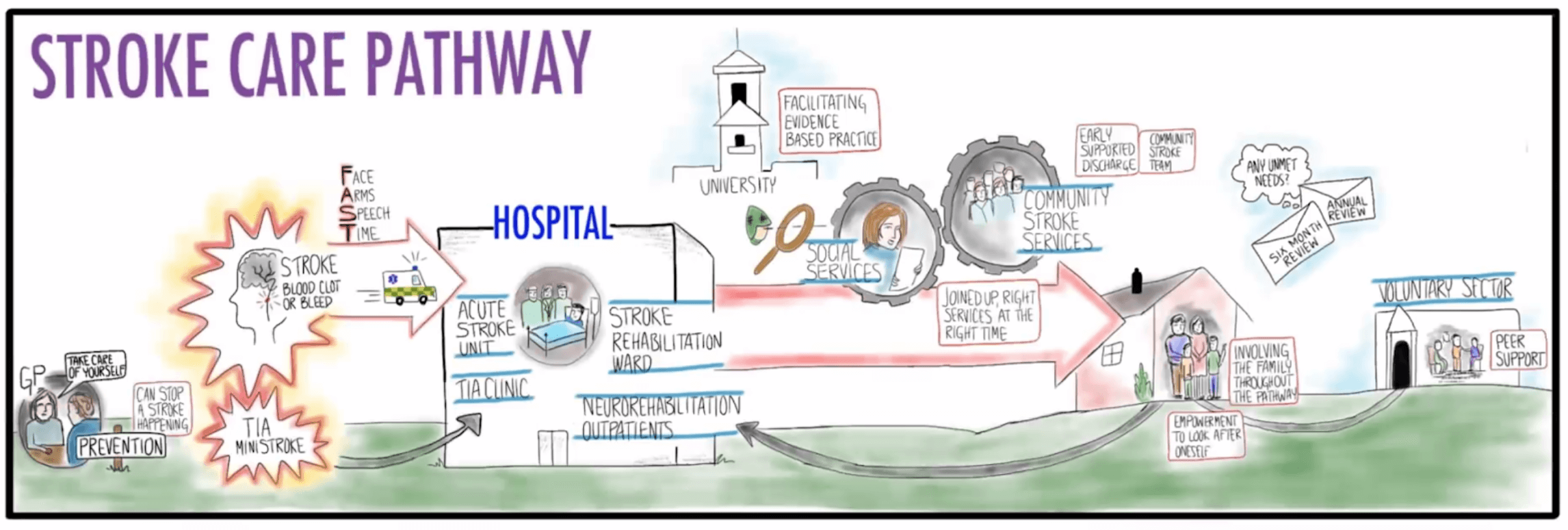
Recently, the Stroke Association led the Stroke Priority Setting Partnership to hear from survivors of stroke, family and friends of the survivor, and health professionals involved in the survivor’s care2. The aim was to understand and bring awareness to the key priorities surrounding stroke at all stages, ranging from stroke prevention all the way to long-term care.
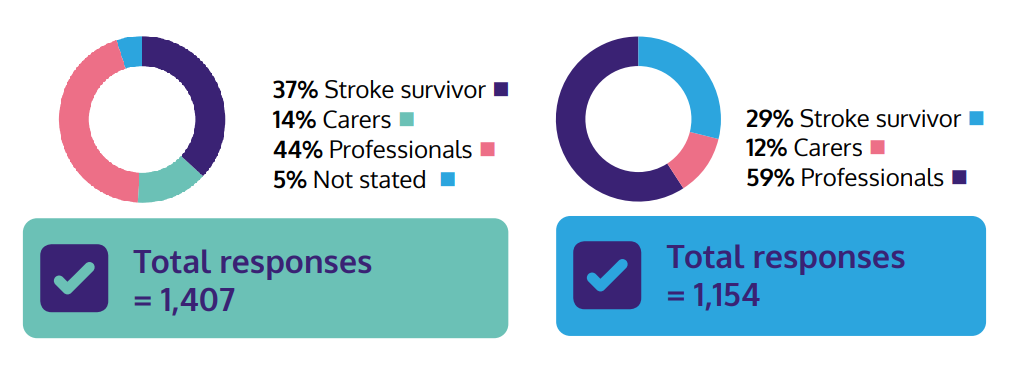
Initially, unanswered questions about stroke were collected from surveys of stroke survivors, carers and professionals. These questions were then filtered and combined to form 93 questions. A second round of surveying was then conducted to select the most important questions from the reduced list. A breakdown of the respondents at each of these stages can be seen below:
The results of this process were two lists of 10 priority areas in:
- Prevention and acute care of stroke
- Rehabilitation and long-term care
In this post, we’ll be focusing on the second list, ‘Rehabilitation and long-term care’.
Why was there a stroke report?

Stroke is not going away
The impact of stroke is growing continuously. The number of people living with the effects of stroke is set to double to 2.1 million by 20353. Reports like this ensure key areas of improvement are highlighted now, so that any future survivors receive the most-up-to-date and effective treatment in their rehabilitation journeys.
Stroke research is underfunded
Stroke currently costs the NHS and social care services £8.6 billion per year4. Despite this, stroke research only receives £30 million public and charity health spend out of a total £2.56 billion (approximately 1.2%)5.
However, even if only £10 million were to be invested into stroke cognitive rehabilitation, almost £725 million could be saved over 20 years, based on estimated savings to areas such as health and social care, formal services, unpaid care, and value of assumed gains in quality adjusted life years6.
It is evident that more investment needs to go towards stroke research, and highlighting the key problems as this report does, gives clarity as to why and where investment is needed.
Those most affected by stroke need a voice
Stroke is a complex condition.
Many people are involved when a stroke occurs, including the survivor, their family, friends, and medical professionals. By hearing from these people directly to develop priority areas, researchers can ensure that resources are spent on areas that matter most and will make the biggest differences to people’s lives.
So, what are the biggest priorities?
If you want to see the full list of priorities for rehabilitation and long-term care, you can find them at the end of this article. Read on to view a summary and brief description of the different priorities relating to the management of stroke and the care processes involved.
Effects of stroke
When a stroke occurs, many parts of the brain can be affected, resulting in potentially a wide range of lasting effects for survivors.
It is important to note that each stroke case is unique. Any combination of effects could occur in a stroke survivor, with differing severities from case to case. Even in the situation where two survivors were to have the exact same effects from a stroke, factors such as their postcode, the number of people in their support group, and access to local resources could play a huge role in shaping the survivor’s day-to-day lives and long-term recovery.
The top four priorities for rehabilitation and long-term care all relate to specific effects resulting from stroke, respectively:
- Mental and emotional (psychological) problems
- Thinking and memory (cognitive) problems
- Impaired communication abilities
- Fatigue
The key findings related to these effects have been summarised below:
Focusing on the most significant questions
For each of the effects above, key questions were identified, including:
- How does this effect impact the lives of people affected by stroke?
- How often does this effect occur?
- What can be done to improve the wellbeing of patients?
Whilst the above lists for the effects of stroke and key questions are not exhaustive, it is clear that survivors, carers and clinicians want to see improvements in the assessment and treatment of these issues in particular.
With more information, better specialised care and rehabilitation plans can be generated by medical professionals. Furthermore, by considering the impact on a case-by-case basis, appropriate support can be provided to improve the overall wellbeing of the stroke survivor, such as by helping with returning to work or assisting financially.
Availability of care to manage the different effects
The priorities also show that there are still many questions regarding the best interventions for reducing the impact of the effects for the survivor.
The NHS has an ambition to ensure patients are able to receive consistent high-quality care throughout the week, including weekends. However, for stroke survivors, the current advice as stated in the Stroke Guidelines is to receive 5 therapy sessions a week for 45 minutes each, despite research indicating higher repetitions lead to improved patient outcomes. For example, more frequent speech therapy sessions which continue over the weekend correlates to better short and long term recovery prospects for communication.
To more closely align with the view of ‘providing care when it is needed, not when it is available’, changes should be made to consider the needs of stroke survivors and offer more care if required in certain situations. In the words of Professor Rustam Al-Shahi Salman (British Association of Stroke Physicians President and Steering Group member), “Research is needed to address the many uncertainties about how stroke prevention, treatment, and recovery can be further improved.”
More effort needs to be given to identify the most effective provision of rehabilitation sessions, ensuring that patients are able to increase the frequency and duration of rehabilitation in a cost-effective manner.
Tracking treatment efficacy
Another topic addressed in the report is that there is still great uncertainty regarding which assessments and interventions are best to manage the various effects of stroke.
To actually identify the best rehabilitation strategies, evidence is needed. However, it is hard to track progress and get evidence during rehabilitation when there is little or no data available. According to Jennifer Crow (Chair of Royal College of Occupational Therapists Specialist Section, Neurological Practice Stroke Forum and Steering Group member), “As an occupational therapist in stroke, my colleagues and I rely on research evidence to guide treatment and care for our stroke patients. But there are gaps in the evidence.”
If evidence can be obtained to track progress, comparing efficacies of treatments in different situations becomes easier, and so there will be more confidence when treating a patient that they are receiving the best care.
Care
Apart from the issues surrounding the effects of stroke, there are also priority areas regarding the care processes for stroke survivors.
Many individuals are involved in the care of a stroke survivor. It is important to ensure that everyone contributes effectively to the survivor’s rehabilitation journey, and that everyone is involved in the further development of stroke care.
Connecting the care teams
It’s crucial to connect the people supporting the stroke survivors with the stroke care team.
Guidance on providing support to stroke survivors can be passed from the professional care team to the home support team. Other individuals, such as volunteers and stroke liaison workers should also receive sufficient training and support to adequately provide care to stroke survivors.
By implementing these changes and training a patient’s support network, informal caregivers are able to go beyond basic care and help improve long-term patient outcomes.
Ensuring accessibility of services
Community stroke services need to meet the needs of all stroke survivors.
When organising home and community-based rehabilitation, there are often significant variations in the level of support available across the UK. Furthermore, provisions should be made to provide effective care for patients regardless of factors such as stroke severity, age, or presence of other health conditions.
By ensuring rehabilitation services meet the needs of everyone, more survivors would be treated and would feel less isolated, in turn improving a greater number of lives in the long-term.
Receiving feedback
Lastly, stroke survivors and their carers need to be consulted, and their feedback needs to be taken into consideration.
The question “What can be done to improve the stroke survivor and carer experiences?” is very important, and is probably the most useful in making advancements in stroke care in the future. The best way to answer this and make developments is to find out from the people who experience everything first-hand.
Through initiatives such as the Stroke Priority Setting Partnership, in which feedback is directly obtained from people, prevalent concerns across the whole community can be addressed and rectified. This can also be done on a local scale by encouraging patients to express their views on their experiences in clinics, improving local care services in the future.
What’s next?
There are many additional priority areas that didn’t make the top 10. In the future, these priorities may enter the top 10 as other issues get addressed, so regular review is important to track progress and see changes in sentiment in the stroke community.
For now, the Stroke Association has taken the priority areas and has called on the following action points to improve care throughout all stages of the stroke care pathway:
- More investment in stroke research from funders and research institutes
- Greater focus on priority areas and involvement of people affected by stroke from researchers
- Investment increase and enablement of stroke research to address priorities by health and social care policy and decision-makers
- Advocation for priority areas and involvement in research by people affected by stroke and professionals
Where does neumind fit into all of this?

With Alfred, we’re providing a modern and intuitive tool which aims to address many of the priority areas surrounding the rehabilitation and long-term care of acquired brain injury (including stroke) survivors.
We provide a way of directly connecting the survivor to their support group, including family, friends and medical professionals, allowing them to send reminders or other rehabilitation exercises remotely. By making use of our data-driven and analytical software, insights can be generated for each individual survivor, allowing clinicians to analyse the efficacy of rehabilitation procedures. The clinician can then implement any necessary changes to the treatment quickly, tailoring the care to each survivor.
Best of all, we are very open to suggestions and guidance from the community, so if there’s any way in which you think Alfred can be improved, let us know!
Thanks for reading!
Full list of priorities
- Mental and emotional (psychological) problems can be caused by stroke/TIA. How common are psychological problems and what impact do they have on the lives of people affected by stroke (including the children of stroke survivors); what factors and interventions can best prevent psychological difficulties, support adjustment, and improve motivation, wellbeing and engagement; how cost-effective are these interventions and how can they be made available to people affected by stroke?
- Thinking and memory (cognitive) problems can be caused by stroke. What is the best way to assess for and understand the impacts of these, and track progression in all areas of cognition — including using standardised measures — across the stroke pathway; what and how can interventions and services involving multidisciplinary teams and families be made accessible; and how can information on these problems be provided?
- Stroke can affect communication abilities, such as reading, speaking and listening as well as social and related ‘thinking’ skills (cognitive communication disorder). What are the effects of, and best assessments and interventions for, the range of communication difficulties in stroke survivors?
- People with stroke/TIA can experience fatigue. How common is fatigue; what and why are there various types, causes/triggers and experiences of its effects? What are the best ways to recognise, reduce, treat and self-manage fatigue — including in young stroke survivors and for all types of stroke, including subarachnoid haemorrhage — to minimise the impact on recovery and life after stroke?
- How can community stroke services best be resourced and organised in all regions to provide effective home/community-based rehabilitation that meets the needs of all groups of stroke survivors such as ethnic groups, young people, stroke severities and those with multiple health conditions?
- What and how common are the long-term impacts of stroke on abilities necessary for everyday life; what interventions can be made available to facilitate these abilities, and how? For example, impact on and interventions including education, assessment, treatment and support for return to work, driving, relationships and financial wellbeing.
- What is the best time, place and amount of therapy (e.g., speech and language therapy, physiotherapy, occupational therapy) to get the best outcomes for stroke survivors, and is this different than advised in the Stroke Guidelines (5 times a week for 45 minutes)?
- How can people supporting stroke survivors work best with the stroke care team, and what personalised training and support is available for carers to enable them to support stroke survivors and their recovery, including those with communication, cognitive and engagement difficulties? For example, the roles of family members, volunteers, stroke liaison workers and young carers.
- What are the best interventions including exercise to improve strength and fitness, promote recovery and prevent further stroke in stroke survivors?
- What do stroke survivors think and feel works well, or needs improvement as they move through the stroke pathway, including the intensity of rehabilitation? What can be done to improve the stroke survivor and carer experiences?
References
- https://www.nejm.org/doi/full/10.1056/NEJMoa1804492
- https://www.stroke.org.uk/sites/default/files/research/stroke_priority_setting_partnership_full_report.pdf
- https://academic.oup.com/ageing/article/49/2/277/5707457
- https://academic.oup.com/ageing/article/49/2/270/5679684
- https://hrcsonline.net/reports/analysis-reports/uk-health-research-analysis-2018/
- https://www.stroke.org.uk/sites/default/files/economic_impact_of_stroke_report_final_feb_2020_0.pdf
- https://www.nottingham.ac.uk/research/groups/strokerehabilitation/people/ossienewell.aspx